Introduction
Tuberculosis (TB) and is the leading infectious cause of death in adult's worldwide.TB can have a wide variety of presentations manifestation. Hematological manifestations of tuberculosis have different forms and one of the rare associated is TB with isolated thrombocytopenia. ITP is relatively common autoimmune bleeding disorder.. However, ITP is very rarely associated with TB with only a few cases reported. Isolated Thrombocytopenia in TB is multifactorial and could be explained by different mechanisms as follows Immune-mediated platelet destruction through antiplatelet antibodies as mycobacterium TB may share antibodies with platelets or platelet-associated immunoglobulin, Tuberculosis-induced hemophagocytosis, Defective platelet production due to bone marrow (BM) infiltration, Hypersplenism, intravascular coagulation, anti-tuberculous treatment (ATT) induced thrombocytopenia.
Methodology
We reviewed the literature using PubMed, google scholar and English language articles only.
We have included all the reported cases of tuberculosis and immune thrombocytopenia if it is associations or initial presentations using the keyword: tuberculosis. Pulmonary tuberculosis, immune thrombocytopenia, Idiopathic thrombocytopenia purpura and we excluded drug induced thrombocytopenia. Our review identified forty-two cases in total, in our review Baseline and clinical characteristics are provided.
Results
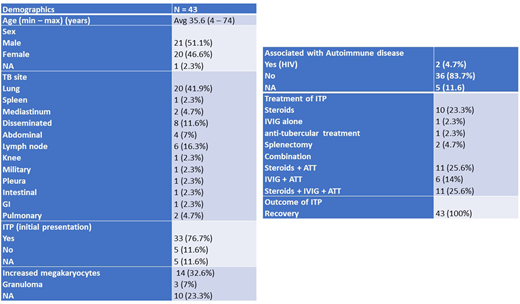
Of the forty-two cases identified, more than one quarter of cases (n=12) were from India; the remainder of the reported cases from thirteen different countries. Gender was nearly equally distributed (males n= 21, females n=20, one case unknown); age ranged from 4 to 74 years.
The most reported sites of TB as follows; lung (n=20), disseminated (n=8), lymph nodes (n=6), abdomen (n=4), mediastinum (n=2), spleen (n=1) and knee (n=1).
Bone marrow aspiration and biopsy done in 27 cases, three of them (7%) found granuloma and 14 (32%) found to have normal to hyprecellular marrow with increased number of megakaryocytes. Of the forty-two cases, ITP was the first presentation of TB with or without typical TB symptoms and signs in more than three quarters of the cases (n=33), while ITP was discovered in TB patients in routine investigations without obvious bleeding symptoms or signs in only four cases. Hemorrhagic symptoms were reported in most of the cases (n=31), skin manifestations (petechiae/purpura/ecchymosis) being the most common (n=28).
The therapeutic approach to TB-associated ITP showed significant heterogeneity with Anti tuberculous treatment and first- and/or second-line treatment for ITP given with or without platelets transfusion.
Most of the cases (n=36) achieved full recovery with Anti-tuberculous treatment(ATT) and IVIG ± Steroids. Of the 42 cases, six cases were treated with blood and platelet transfusion for thrombocytopenia which did not normalize the platelet count as thrombocytopenia as expected as this is most likely an immune mediated phenomenon.
Conclusion
Unfortunately, there are no clear guidelines for management of TB-associated ITP and is anecdotal or observational at best. This highlights the importance of conducting prospective and standardized studies in the future. We found that Anti tuberculous treatment could have play pivotal role in management of ITP in TB Patients.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal